When women find themselves diagnosed with polycystic ovarian syndrome (PCOS), one of the first treatment options they’re often offered is the pill. And, it’s no surprise – hormonal birth control is the most common treatment for PCOS within conventional medicine.
But, it may not be the best.

If you haven’t read my first post on understanding PCOS (here) or my second on PCOS and insulin resistance (here), be sure to check those out first!
When it comes to the pill and its relationship with polycystic ovarian syndrome, there is a lot to unpack. That’s why I’ve put together the six main points you should know and consider before getting started on the pill to manage your polycystic ovarian syndrome.
Do I think the pill isn’t a good choice for anyone? Of course not – all treatment options work differently for different patients, but understanding the risks and benefits of each is important when making the decision on which is best for you.
If you haven’t already, be sure to start out with parts one and two in my PCOS series, covering the basics of PCOS and how insulin and PCOS are connected (something that will be good to know when we’re talking about the pill).
The pill is often prescribed for women with PCOS since the combination pill (with synthetic estrogen) has been shown to be helpful for reducing acne and hirsutism. When it comes to androgens, though, the main issue is that it only works for as long as you are taking the pill.
And it’s important to recognize that the pill doesn’t come without risks. The combined pill with synthetic estrogen and progesterone increases your risk of breast cancer. The pill also increases the risk of developing a blot clot 3-4x and even more depending on your genetics.
The progestin only pills can be problematic because synthetic progestin is actually more like testosterone than it is progesterone. This can make androgen symptoms worse for some women.
One of the biggest downsides of the pill is that it can worsen insulin resistance, which is a main driver of PCOS for most women. This is a huge concern since the pill is often one of the first lines of treatment for women with PCOS that don’t want to have kids.
We need to think about the long term impacts that this can have on women with PCOS. There’s already an increased risk of heart disease. Increasing insulin resistance, inflammation, and reducing carbohydrate tolerance could exacerbate that.
The pill is also associated with an increase risk type 2 diabetes in healthy women, which could be even greater for those with PCOS. Unfortunately, there haven’t been any studies done on women with PCOS (which blows my mind considering insulin resistance), but if you are struggling with insulin resistance, the pill could be making it worse and doing more harm for your PCOS symptoms than good.
Research has shown that the pill increases CRP, an inflammatory marker, by 39%. This is problematic because inflammation can lead to other metabolic issues and is a main driver of symptoms for many with PCOS.
The other way that the pill can increase inflammation is the stress response that it causes. The pill (and any other hormonal BC) is a stressor on the body. The influx of hormones daily causes a stress response. Your brain is alerted to stress, tells the adrenal glands there’s inflammation, and then cortisol is released. This happens over and over and eventually the brain and adrenal glands don’t speak in a functional way. This causes adrenal dysfunction and a low grade inflammatory response in the body.
More inflammation can lead to more insulin resistance, higher androgens, and metabolic chaos in those with PCOS. This is why it’s important to weigh the risks vs. benefits with the pill. And also why I only think it should be used to prevent pregnancy, not “fix” hormonal imbalances.
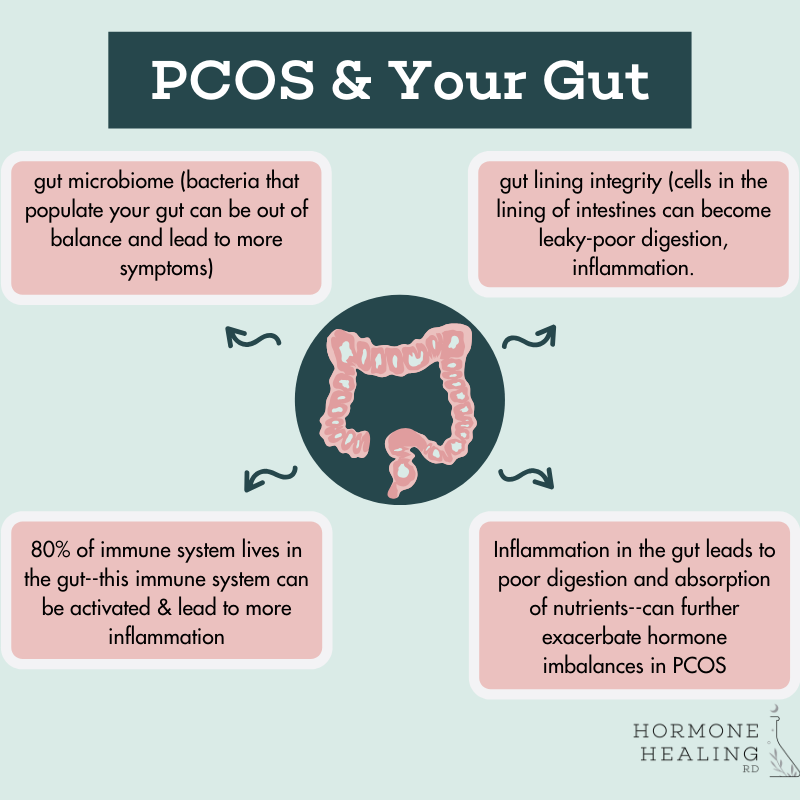
Like we just mentioned, women with PCOS have higher levels of inflammation, which can impair gut health and function. They also have an imbalance of gut bacteria and tend to have a deficit of beneficial bacteria. The integrity of the gut lining can be damaged from inflammation, pathogens, and lead to poor absorption of nutrients.
If you add the pill into the mix, this can lead to further gut bacteria imbalances and more inflammation. All of that can impact insulin resistance and hormones, making PCOS symptoms worse.
The pill (both combined and progestin only) can negatively impact thyroid function. Why is this a concern for women with PCOS?
It’s estimated that about 25% of women with PCOS have hypothyroidism, although I see it much more frequently than that. This isn’t surprising since a number of studies have found that insulin resistance and metabolic syndrome reduce the conversion of T4 (inactive form of thyroid hormone) to T3 (active form of thyroid hormone) and increase reverse T3 (puts the breaks on conversion).
The pill also increases insulin resistance, like we discussed, and depletes the nutrients selenium, zinc, and B vitamins, which are all essential for thyroid function. Lastly, the pill increases Thyroid Binding Globulin (TBG), which binds to thyroid hormone making it unavailable for use by cells. Every cell in our body requires thyroid hormone.
Women with PCOS are nearly three times more likely to suffer from anxiety and depression than women without PCOS.
What does this have to do with the pill?
There continues to be emerging research on the link between the pill and depression. One Canadian study found that women who took the pill as teenagers are 3 times more likely to experience depression later in life, even after they discontinue use of the pill. There’s also research exploring the link between nutrient deficiencies from the pill and depression, like vitamin B6. More research needs to be done on whether or not supplementation helps, but this is an area of emerging research that is important for anyone using the pill as a medication option, both with PCOS and without.
Women with PCOS deal with a number of symptoms from their condition like hirsutism, difficulty losing weight, and infertility that impact their quality of life, not to mention the fact that most women with PCOS deal with anovulatory cycles and low progesterone, which is our calming hormone. These factors can have effects on overall wellbeing and quality of life, and can exacerbate symptoms associated with depression and anxiety.
Despite what many doctors may believe, the pill, in my opinion, is for one thing – preventing pregnancy. While many people with PCOS do well on the pill, so many also struggle, both from the side effects they experience and due to the lack of information provided to them by their doctors. My goal isn’t to make you (or anyone with PCOS) stop the pill. It’s only to share other information that can help you make an informed decision on whether or not it’s right for you.
The first step in figuring out how to control your symptoms is understanding the root cause of your condition. the Hormone Healing RD nutrition team can help you do that. i’m currently taking on 1:1 clients. if you’d like to explore what it would be like to work together and if we are a good fit, fill out this form to get more details!
