It’s a term you may have heard before, but with the amount of information swirling around the internet, it can be hard to define. And it’s understandable that you feel confused, overwhelmed, or downright lost when trying to understand it.
It’s polycystic ovarian syndrome, or PCOS, and it affects nearly one in every ten women of child bearing age.
Understanding PCOS is the first step in getting control of your condition, and that can mean learning a lot about things like cysts, insulin resistance, and the right nutrition and supplement options for you and your PCOS. In this four part series, we cover it all, from what PCOS is and the different types, to the relationship between PCOS and insulin, and how they’re all supported by your choices you make about your nutrition.
What is PCOS?
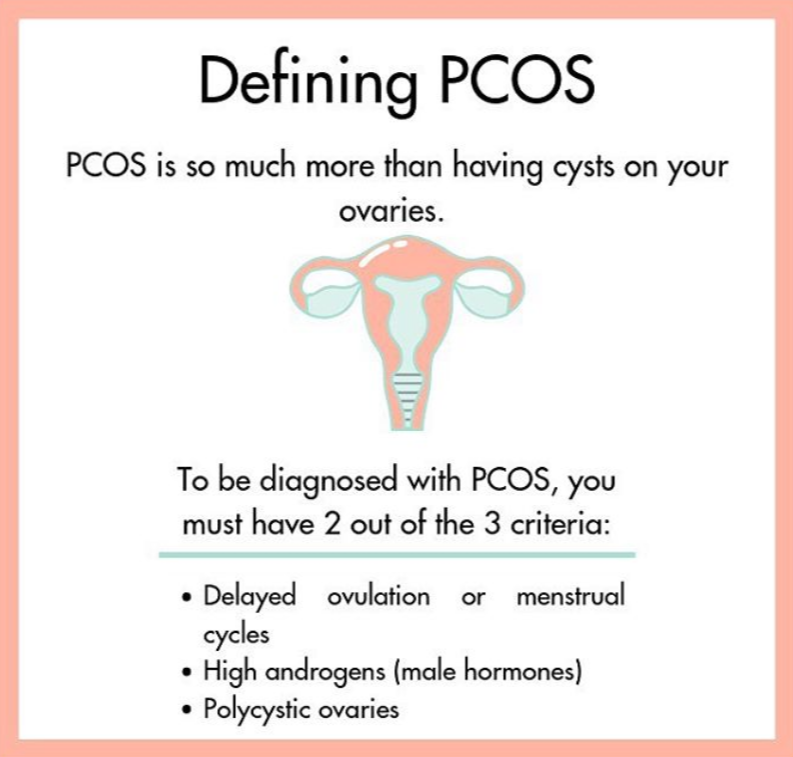
Polycystic ovarian syndrome is a “common health problem caused by an imbalance of reproductive hormones” that can lead to the development of cysts on the ovaries and potential infertility in women. PCOS, though, is so much more than having cysts on your ovaries and in my opinion (and the opinion of many!), is a disease that needs a new name. As we’ve continued to learn more about this condition, we now know you can no longer diagnose PCOS simply by seeing cysts in an ultrasound.
There are actually 3 criteria that were created by leading experts in 2003. This is typically known as the Rotterdam criteria and, in order to meet the criteria for PCOS, you actually only have to have two out of the three. This is what created the types of PCOS that we’ll cover later, but is great for understanding why PCOS for one woman isn’t the same as another.
Here are the criteria:
When it comes to cysts, there can also be a great deal of confusion surrounding the presence of cysts found on an ultrasound. Not all cysts found on an ultrasound are ‘true’ ovarian cysts, and many otherwise healthy women will develop cysts separate from PCOS.
Just like PCOS, there are different types of cysts that may be found on ultrasound.
What Causes PCOS?
There are a number of things that contribute to PCOS, but when it comes down to it, Polycystic Ovarian Syndrome has a few main contributing factors, including high androgens and elevated insulin. High androgens are what stalls the growth of the follicles and delays ovulation. Anovulatory cycles are what then lead to hormonal imbalances and, subsequently, symptoms of PCOS.
Chronic low grade inflammation that occurs with PCOS causes the body to be less sensitive to insulin. This means we need to release more insulin in order to get the same amount of energy in our cells, which can be damaging not only to our ovaries but also to the rest of our body.
These two factors are also connected. High insulin levels irritate our ovaries and cause them to release more androgens. Then, the androgens cause the anovulatory cycles, making the process cyclical and tough to beat.
PCOS is truly a condition of high androgens. Just like with any disease, it’s important to rule out other conditions that may be causing your symptoms. For PCOS, that means ruling out other conditions that can cause hormonal imbalances such as high androgens or other symptoms in polycystic ovarian syndrome.
Conditions that also cause high androgen include high prolactin, hypothyroidism, and pituitary or adrenal diseases, though this is rare. Androgens can also be high after getting off of birth control, known as ‘Post Pill PCOS’, or when coming off of certain psychiatric medications.
Outside of the medical conditions that can cause high androgens, there are also other reasons you may have higher than normal androgens outside of (or in conjunction with!) PCOS. These include chronic stress, inflammation, nutrient deficiencies, sluggish liver, low stress hormone binding globulin, poor diet, and kidney issues.
Types of PCOS
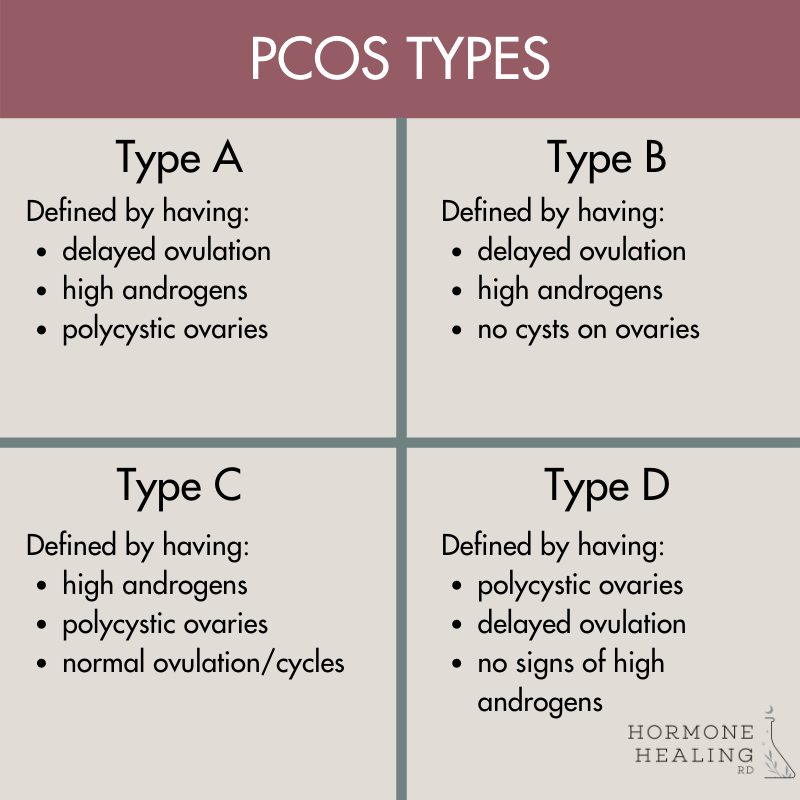
One of the biggest challenges when it comes to understanding PCOS is knowing that no two women are exactly alike and, because of that, neither are their diseases. While everyone experiences PCOS differently, there are four main types of polycystic ovarian syndrome that most women fall into.
Wrapping It Up
It’s easy to see why there is so much confusion surrounding polycystic ovarian syndrome, and why women can feel lost when looking for answers for their symptoms. The good news is that, with understanding, there are options for managing PCOS along with the help of a qualified provider.
The first step in figuring out how to control your symptoms is understanding the root cause of your condition. the Hormone Healing RD nutrition team can help you do that. i’m currently taking on 1:1 clients. if you’d like to explore what it would be like to work together and if we are a good fit, fill out this form to get more details!
In our next part, we’ll talk about insulin and its effect on PCOS. Find the link to the next post here.
