It’s easy for people to misunderstand polycystic ovarian syndrome, or PCOS, as simply a disease of the ovaries. But, as we know, it’s so much more than that (and, if you don’t know, be sure to check out part one in our Understanding PCOS series here).
PCOS is identified by three main criteria – delayed ovulation or menstrual cycles, high androgens, and polycystic ovaries – and is broken down into four subtypes. Each type has specific criteria, but many have something in common, and that is insulin resistance.
Insulin resistance is what happens when we have too much insulin in our bodies. While we need insulin – it tells our cells to open up and take in the glucose we’ve broken down from our food – insulin resistance can cause our bodies to stop responding to the insulin we have, leading us to produce more and more until, one day, our bodies stop responding all together. When our bodies stop responding, we can develop weight gain, heart and bone health issues, and, eventually, diabetes.
Insulin resistance can be a challenging condition to understand, however there are a few common signs of insulin resistance, including fat gain around the belly, difficulty losing weight, skin tags, and dark pigmentation at the folds of your skin on the neck. Weight itself isn’t a predetermining factor, as people at a healthy weight can also have insulin resistance.
But how does this relate to PCOS?
While not all types of PCOS are driven by insulin resistance, most types have some degree of insulin resistance occurring. This can be a major factor in managing your symptoms of PCOS, as figuring out what is at the root of your personal condition is one of the first steps in getting PCOS under control.
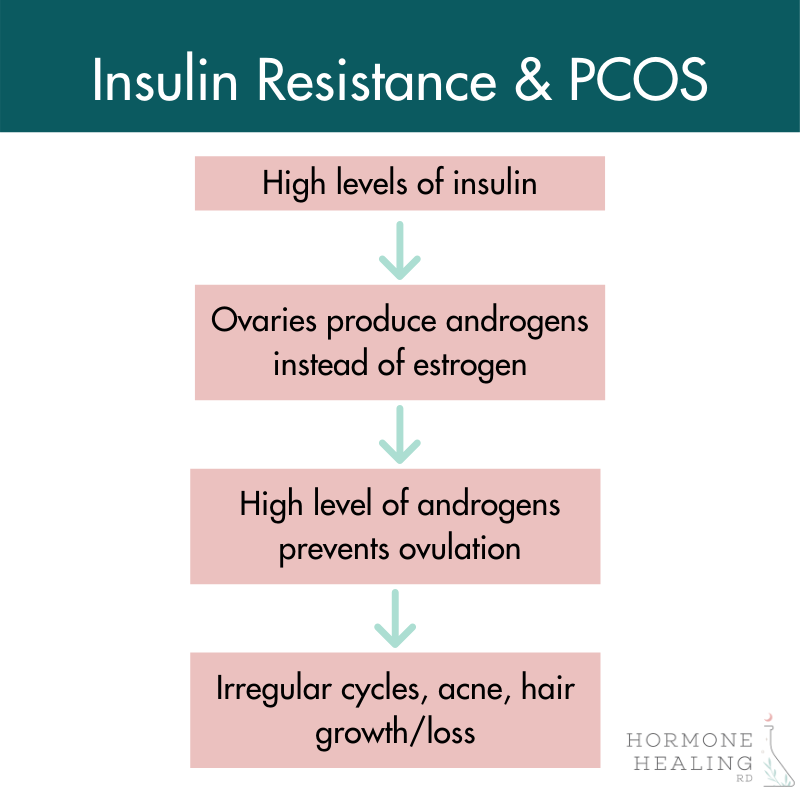
High levels of insulin in the body irritate your ovaries, causing them to produce more androgens like testosterone, instead of estrogen. Your pituitary gland also reacts to high levels of insulin by making more luteinizing hormone, or LH. Excess levels of insulin also impact an important compound called steroid hormone binding globulin, or SHBG. Insulin can decrease the levels of SHBG, leading to a rise in testosterone, one of the key criteria (high androgens) in PCOS.
Identifying Insulin Resistance
How do you know if you have insulin resistance?
Thankfully, there is a way to determine if you have insulin resistance and help you further understand your PCOS in an actionable way. Lab testing is available to help identify insulin resistance. Here are three tests you can have done in order to help identify insulin resistance.
Managing your Insulin Resistance
Once you have identified your insulin resistance, there are ways to help manage and improve your insulin sensitivity before the condition progresses further or, potentially, develops into a more serious condition like diabetes. Here are my seven top tips for managing your insulin resistance.
Most importantly, managing your insulin resistance (and, subsequently, your PCOS) is about nourishing your body and experimenting to find what works best for you. Sustainability in managing your symptoms is key, so make sure to identify options you can keep up long term.
Treating Your Insulin Resistance
In addition to the tips above, there are other ways to manage your insulin resistance, especially as it relates to your polycystic ovarian syndrome. Some treatments may be more conventional, such as medication, while other more natural, less invasive options are available as well.
Metformin is a prescription medication (glucophage) that prevents the liver from breaking down stored glucose and putting it into the bloodstream. This reduces the breakdown of fats and encourages our cells to take up more glucose. Metformin has also been shown to alter a patient’s gut bacteria, but in a good way – it can help bump up the metabolism boosting types of bacteria found in the gut which could explain why it’s helpful for insulin resistance.
While this drug can be a great option for some patients with insulin resistance, Metformin does come with certain risks and side effects. It has the potential to deplete vitamin B12, and can cause nausea, diarrhea, vomiting, bloating, abdominal discomfort, and lactic acidosis, a rare but fatal side effect. Understanding the risks and benefits of this medication (and any medication or supplement) is important when setting up your treatment plan.
Other options, however, do exist for the treatment and management of insulin resistance related to your PCOS. One of these options is inositol, a sugar alcohol that is part of the Vitamin B family. Inositol works by supporting specific signaling pathways that reduce insulin resistance, and by reducing overall testosterone. This helps support ovarian function, which is a huge win for so many with PCOS. Inositol is one of the most researched supplement options available for PCOS, and comes with few potential side effects, including loose stools and upset stomach, which are rare and are often related to incorrect dosing. Be sure to speak with your healthcare provider regarding any changes to your current medications or new supplements.
In addition to inositol, many women with polycystic ovarian syndrome benefit from supplementation with D-chiro-inositol. Women with PCOS have been found to excrete six times more D-chiro-inositol, a type of inositol involved in insulin signaling, than women without PCOS, and losing more could be related to poor insulin sensitivity. While D-chiro-inositol has been found to be especially beneficial for egg and embryo quality, you do need to be careful in the amount of this supplement you take. Be sure to work with a healthcare provider before beginning a supplement regimen.
At the end of the day, you need to identify your current health markers, nutrition, lifestyle, and what you’re willing to change in order to make the best decision regarding medication or supplementation. Taking medications is not a ‘bad’ choice – in fact, it is sometimes necessary! – but having the education and information to make the best decision possible in conjunction with you health care practitioner is my main goal.
Wrap it up
Insulin resistance may not be a concern for every woman with PCOS, but for many, it is. Understanding and managing your insulin resistance can be part of your overall plan for managing your polycystic ovarian syndrome and, in the end, improving your quality of life.
The first step in figuring out how to control your symptoms is understanding the root cause of your condition. the Hormone Healing RD nutrition team can help you do that. i’m currently taking on 1:1 clients. if you’d like to explore what it would be like to work together and if we are a good fit, fill out this form to get more details!
